Acute Coronary Syndrome (Oxford Handbook)
Acute coronary syndromes (ACS)
ACS includes unstable angina and evolving MI, which share a common underlying pathology—plaque rupture, thrombosis, and inflammation. However, ACS may rarely be due to emboli or coronary spasm in normal coronary arteries, or vasculitis. Usually divided into
or new onset LBBB—what most of us mean by acute Ml; and ACS without ST segment elevation —the ECG may show ST-depression, Twave inversion, non-specific changes, or be normal (includes non-Q wave or subendocardial MI). The degree of irreversible myocyte death varies, and significant necrosis can occur without ST-elevation. Cardiac troponins (T and 0 are the most sensitive and specific markers of myocardial necrosis, and have become the test of choice in patients with ACS (see below).
Risk factors Non-modifiable: age, female, family history o IHD (MI in first degree relative
operative hypotension or oliguria, acute confusional state, stroke, diabetic hyperglycaemic states.
Signs Distress, anxiety, pallor, sweatiness, pulsefi or . [Pt or , 4v heart sound. There may be signs of heart failure (9 lvP, 3 heart sound and basal crepitations) or a pansystolic murmur (papillary muscle dysfunction/rupture. VSD). A low-grade pyrexia may be present. Later, a pericardial friction rub or peripheral oedema may develop.
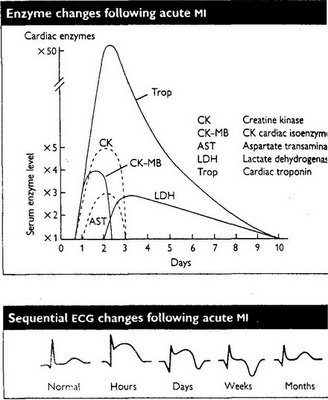
Tests ECG: Classically, hyperacute (tall) T waves, ST elevation or new LBBB occur within hours of acute Q wave (trassmural infarction). T wave inversion and the development of pathological Q waves follow over hours to days. In other ACS: ST-depression, T-wave inversion, non-specific changes, or normal. ln 20% of Mls, the ECG mcy be normal initially.
CxR. Look for cardiornegaly, pulmonary oedema, or a widened mediastinum (laortic dissection). Don’t routinely delay Rx whilst waiting for a CXR.
Blood: FBC, U&E, glucose 9, lipids ,cardiac enzymes (cK, AST, LDH, troponin) , as is found in myocardial and skeletal muscle, It is raised in: MI: after trauma (falls, seizures); prolonged exercise: myositis: Afro-Caribbeans: hypothermia: hypothyroidism. Check CK-MB isoenzyme levels if there is doubt as to the source (normal CK-M8/CK ratio <5%).>lwk). If normal >6h after onset of pain, and ECG normal, risk of missing MI is tiny (0.3%). Peak post-MI levels also help risk stratification.
Differential diagnois - Angina, pericarditis, myocarditis, aortic dissection, pulmonary embolism, and oesophageal reflux/spasm.
Management - The management of ACS with and without ST-segment elevation varies. Likewise, if there is no ST-elevation, and symptoms settle without a rise in cardiac troponin, then no myocardial damage has occurred, the prognosis is good, and patients can be discharged. Therefore, the two key questions are: is there ST-segment elevation; and is there a rise in tropon n?
Mortality - 50% of deaths occur within 2h of onset of symptom.
Management of acute coronary syndrome
Prehospital - Arrange emergency ambulance. Aspirin 300mg chewed (if no absolute CI) and GTN sublingual. Analgesia, eg morphine 5—10mg iv + metoclopramide 10mg iv (not IM because of risk of bleeding with thrombolysis).
In hospital, Ox, lVI, morphine, aspirin
Then the key question for subsequent management of ACS is whether there is
ST-segment elevation (includes new onset LEBE or a true posterior MI).
ST elevation
• Thrombolysis, if no contraindication, or primary angioplasty
• beter-blocker, eg atenolol 5mg iv unless contraindicated;
• ACE-i Consider starting ACE-i (eg lisinopril 2.5mg) in all normotensive patients within 24h of acute MI, especially if there is clinical evidence of heart failure or echo evidence of LV dysfunction.
ACS without ST elevation
• beta-blocker, eg atenolol 5mg iv unless contraindicated;
• Low molecular weight heparin (eg enoxaparin).
• Nitrates, unless contraindication (usually given intravenously).
• High-risk patients (persistent or recurrent ischaemia, ST-depression, diabetes, troponin) require infusion of a GPllb/llla antagonist (eg tirofiban), and, ideally, urgent angiography. Clopidogrel may be useful in addition to aspirin.
• Low-risk patients (no further pain, flat or inverted T waves, or normal ECG, and negative troponin) can be discharged if a repeat troponin is negative. Treat medically and arrange further investigation eg stress test, angiogram.
Subsequent Mx - Bed rest for 48h; Continuous ECG monitoring.
• Daily examination of heart, lungs, and legs for complications
• Daily 12-lead ECG, U&E, cardiac enzymes for 2—3d.
• Prophylaxis against thromboembolism: eg heparin 5000u/12h SC until fully mobile. If large anterior MI, consider warfarin anticoagulation for 3 months as prophylaxis against systemic embolism from LV mural thrombus. Continue daily low-dose aspirin (eg 75—150mg) indefinitely. Aspirin reduces vascular events (MI, stroke, or vascular death) by 29%.
• Start oral beta-blocker (eg metoprolol - 50mg/6h, enough to decrease the pulse to <60;>4,8mmoLIL1 or LDL >3.2 mmolIL (p706).
•Address modifiable risk foctors: Discourage smoking. Encourage exercise. Identify and treat diabetes mellitus, hypertension, and hyperlipidaemia.
• Exercise EcG. May be useful in risk stratification post-MI after 3—4wks, and in subjects without ST-segment elevation or a troponin rise.
• General advice, If uncomplicated, discharge after 5—7d. Work He may return to work after 2 months. A few occupations should not be restarted post-MI: airline pilots; air traffic controllers: divers. Drivers of public service or heavy goods vehicles may be permitted to return to work if they meet certain criteria., Patients undertaking heavy manual labour should be advised to seek a lighter job. Diet: A diet high in oily fish, fruit, vegetables, and fibre, and low in saturated fats should be encouraged. Exercise: Encourage regular daily exercise. Sex: Intercourse is best avoided for 1 month. Travel: Avoid air travel for 2 months.
Review at 5wks post-MI to review symptoms: Angina? dyspnoea? palpitations?
• If angina recurs, treat conventionally, and consider coronary angiography
Review at 3 months
• Check fasting lipids, Is there a need for a statin?
Comments